Why It’s A Bad Idea To ‘Just Get COVID’

February 04, 2022
Now that the highly contagious Omicron variant is widespread – and because people may experience milder symptoms with Omicron than with previous variants – you may be thinking, “should I just get COVID?”
“It isn’t wise to intentionally try to get infected with COVID-19, even if the Omicron variant may seem like a safer bet than prior variants, including the Delta variant, which was frequently associated with severe illness,” says Cristina Cicogna, M.D. an infectious disease specialist at Hackensack University Medical Center.
“The ‘just get COVID’ idea is based on flawed thinking. We are still learning about the virus that causes COVID-19, because it’s so new. We don’t know how long immunity from an Omicron variant illness may last. We don’t know whether or not having the Omicron variant will provide immunity against other variants that may arise. Choosing to expose yourself to a virus that causes severe illness in some people isn’t a good idea. There are safer ways to get immunity, namely COVID-19 vaccines and boosters.”
If you’re thinking about “just getting COVID,” consider these reasons why you shouldn’t:
You could still get severely sick.
There’s no guarantee that you’ll have a mild case of COVID-19, even if you get the widely circulating Omicron variant. You’re less likely to get sick enough to be hospitalized if you’ve been vaccinated and boosted, but there’s always the chance that the Omicron variant could affect you more severely than you’d expect.
You may infect others and put them at risk.
The Omicron variant is more contagious than previous variants, so it’s likely that you may get other people sick if you get the Omicron variant. And even if you have a mild case of COVID-19 from the Omicron variant, there’s no guarantee that anyone else whom you infect will also have a mild case. By choosing to “just get COVID,” you may put other people at risk of severe illness, including people with chronic health conditions that put them at higher risk of complications, older adults, people who are immunocompromised and children who are too young to be vaccinated.
The Omicron surge is affecting hospitals.
More people have been hospitalized with COVID-19 this January than at the height of the COVID-19 surge last winter. Different hospitals across the country have been overwhelmed by the sheer number of people who are seeking treatment for severe COVID-19. Staff shortages are affecting some hospitals, as well. If you become infected with the Omicron variant, you risk experiencing illness that warrants a trip to the emergency room at a time when emergency rooms are brimming with COVID-19 patients.
Long COVID is a possibility.
Experts are still learning about the Omicron variant, which was first detected in November (and in the U.S. in December). It’s unknown if getting this variant could lead to long COVID – a constellation of lingering symptoms, including brain fog, fatigue, joint pain and shortness of breath – that may last for months or longer. Some people who had milder illness from other COVID-19 variants have developed long COVID, so you may not be immune to long COVID after having mild illness from the Omicron variant.
Next Steps & Resources:
- Meet our source: Cristina Cicogna, M.D.
- To make an appointment with Dr. Cicogna or a doctor near you, call 800-822-8905 or visit our website.
The material provided through HealthU is intended to be used as general information only and should not replace the advice of your physician. Always consult your physician for individual care.
Does the Booster Protect Against Omicron?

The question on everyone’s mind is, does the booster shot protect against the Omicron variant? Hackensack Meridian Health's chief physician executive, Daniel Varga, M.D. shares some insight.
Why We Shouldn’t Treat Omicron Like the Flu or Common Cold

If the omicron variant is more likely to provide milder symptoms, does it really matter how it spreads? The clear answer is yes.

What You Should Know About COVID Vaccines & Menstrual Cycles
Can a COVID-19 vaccine affect a woman’s menstrual cycle? According to a recently published study, here’s what researchers found:

Just Had COVID? Here’s When to Get the Booster
If you’ve recently had COVID-19 but haven’t yet received your booster shot - should you run to your local vaccination site to get it? Our expert shares some guidance on when is the best time to get your booster.

Can the Booster Make You Test Positive for COVID?
Uncertainty about the COVID-19 vaccines has been common since they were first introduced. Our infectious disease specialist answers the latest viral topic in question.
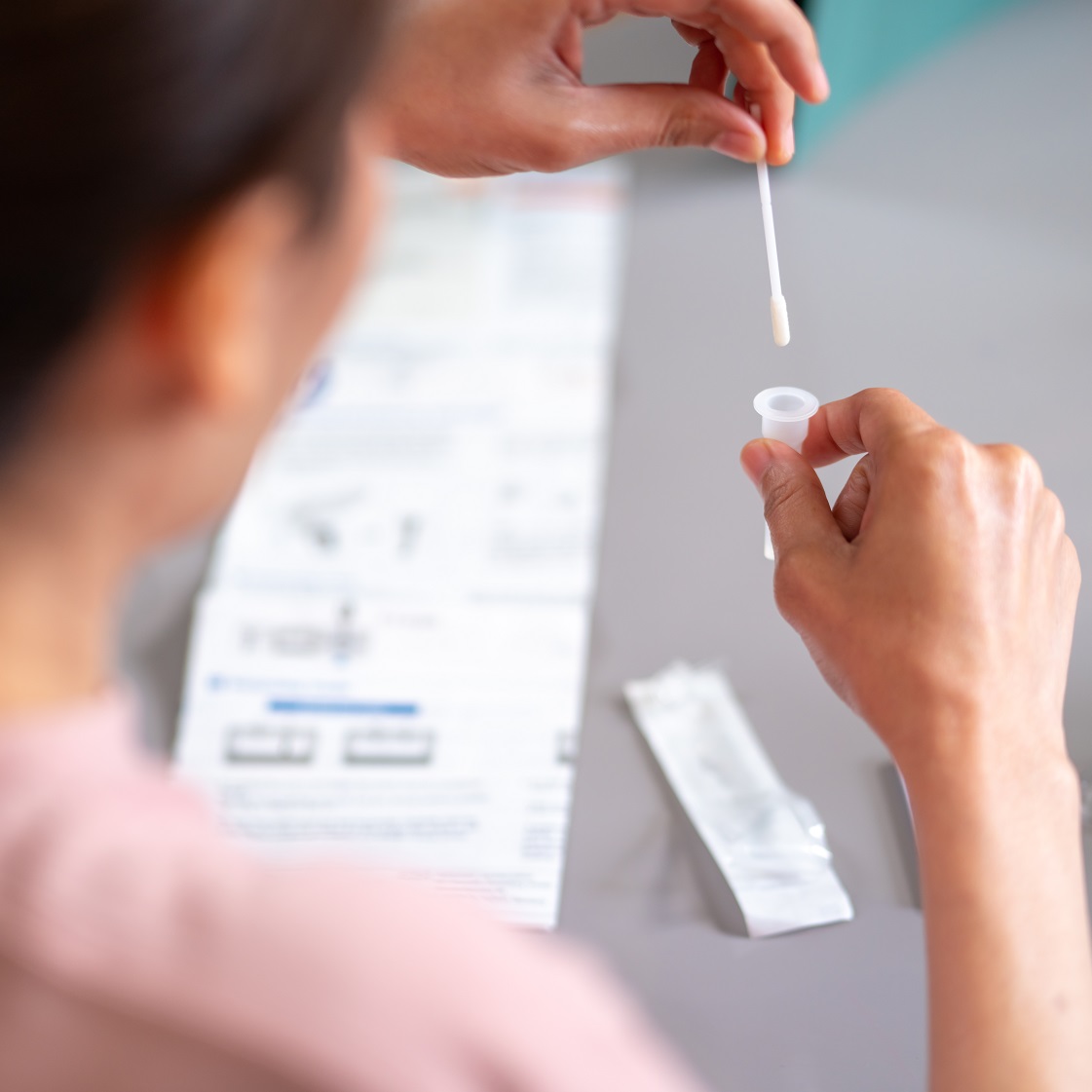
How Accurate Are At-home COVID Tests?
Find helpful answers to the most common questions about at-home COVID tests.