Testicular Cancer Care in New Jersey
Cancer in the testicles happens when cells become abnormal, turn into cancer and form tumors. The testicles, or testes, are the male sex glands that produce sperm and testosterone and are found behind the penis in a pouch of skin called the scrotum.
Our goal when treating testicular cancer is to cure your cancer while preserving your fertility and sexual function. The urologists at Hackensack Meridian Health use the latest techniques to diagnose the exact stage and type of your testicular cancer. We then develop a treatment plan tailored to your lifestyle needs.
If you need surgery, we offer the region’s most advanced robotic surgery for testicular cancer. Our surgeons are among the few in the U.S. who perform robotic RPLND (retroperitoneal lymph node dissection) to minimize muscle and nerve damage. Our robotic approaches offer outstanding outcomes with a faster recovery and return to normal activities.
Testicular Cancer Symptoms
You should perform a regular self exam to check for changes in your testicles or scrotum. Talk to your doctor or see a urologist if you have any of the following symptoms, which may be a sign of cancer or another urology condition:- Painless lump or firm mass in a testicle
- Swelling of the scrotum or testicle, with or without pain
- Feeling of weight or heaviness in the scrotum
- Pain in the testicle or scrotum
- Dull ache in the abdomen or groin
- Changes to the male breast tissue, including tenderness
Diagnosing Testicular Cancer
Testicular Cancer Treatment Options
Robotic and Minimally Invasive Testicular Cancer Surgery
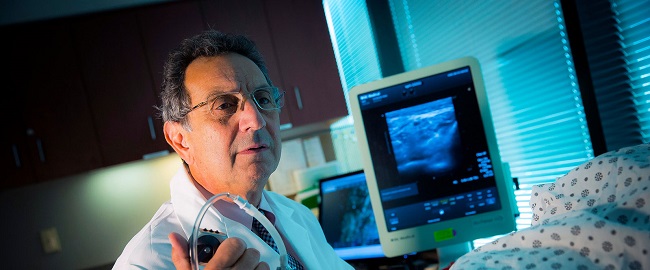
The urologists at Hackensack Meridian Health are recognized worldwide as leaders in robotic surgery. We are highly experienced in robotic and minimally invasive surgeries for testicular cancer
Other Treatments for Testicular Cancer
When it comes to treating testicular cancer, your care team will recommend the most effective treatment for your cancer while preserving as much of your function as possible. We collaborate with specialists across John Theurer Cancer Center on state-of-the-art treatments.
Find a Testicular Cancer Specialist or Care Location
Search our network of testicular cancer specialists or find a care location close to home and make an appointment today.
Find A Testicular Cancer Specialist
Find A Testicular Cancer Care Location
Urological Expertise in New Jersey
The Department of Urology at Hackensack University Medical Center, a nationally ranked program by U.S. News & World Report, is renowned for its high-quality urologic care, including excellence in research and clinical outcomes.
- 6 subspecialties with fellowship-trained urologists
- 2 Joint Commission Disease-Specific Care Certifications in prostate cancer and kidney cancer
- 6 consecutive Magnet designations by the American Nurses Credentialing Center for nursing excellence
Testicular Cancer Research and Clinical Trials
A hallmark of the care we provide is access to a wide range of clinical trials evaluating exciting new treatments for urologic cancers, including studies not available elsewhere. We have a particularly strong program committed to Phase I clinical trials, the earliest phase of assessment of a new therapy in patients. For urologic cancers, we are evaluating novel biological agents as well as immunotherapy options that are changing the field. This offers our patients an opportunity to participate in a clinical trial, bringing the options of tomorrow today. Learn more about clinical trials for urologic cancers.
Frequently Asked Questions

Berkeley Heights Man Spots Testicular Cancer Early


Living Life to the Fullest During Prostate Cancer Treatment